IPSWICH, S.D. – A crisis at the nursing home in Ipswich illustrates the two worst potential outcomes of staffing shortages affecting long-term care facilities across the state: possible nursing home closures and troubling incidents of inadequate resident care.
A shortage of staff was given as one reason that officials for the Avantara Ipswich nursing home said they will close the 40-bed nursing home on May 31, 2022. Challenges related to COVID-19 were also listed.
The closure would leave residents and families searching for new care options, potentially 25 miles away or more. Employees would also face job uncertainty, and the Edmunds County community of 1,000 people about 27 miles west of Aberdeen would see a loss of economic activity. Local municipal leaders have called a public meeting for April 18 to discuss ways to keep the Ipswich home open.
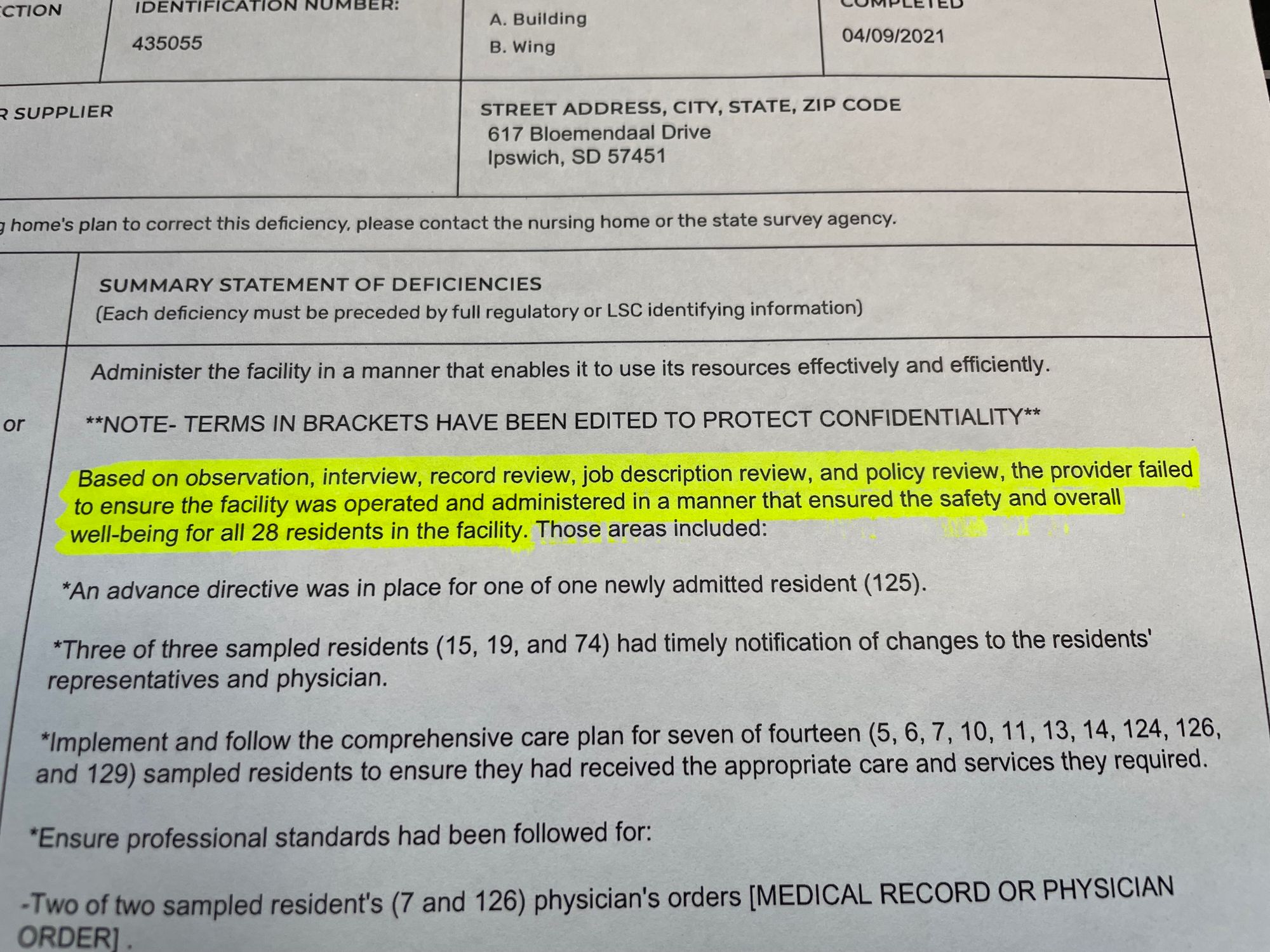
Staffing problems were also identified by the South Dakota Department of Health, which sent inspectors to the Avantara Ipswich nursing home in April 2021. The state compiled a list of 13 code violations in that inspection that required 104 pages to document. Four violations were listed as “Quality of Life and Care Deficiencies.”
According to records from the state health department and the federal government, which were reviewed by News Watch, the April 2021 inspection revealed a facility short on staff, with inexperienced, inefficient management and oversight, and numerous errors or omissions in regard to how residents were cared for.
“The provider failed to ensure the facility was operated and administered in a manner that ensured the safety and overall well-being for all 28 residents in the facility,” the state report concluded.
Legacy Health Care, the Illinois company that operates Avantara Ipswich and 12 other nursing homes in South Dakota, did not return a call or email requesting comment for this story. Legacy administrator Connie Ortega did not return a message, and the director of Avantara Ipswich told News Watch he was unable to comment. A state health department licensing official also declined an interview request from News Watch.
Update from April 28, 2022 – Attempt to save Ipswich home fails
A proposal to keep open the Avantara Ipswich nursing home has failed due to time constraints and inability to raise enough money to buy and operate the facility.
The goal for Ipswich community members was to raise $500,000 so the building could be purchased from Avantara and operated after.
At an April 18 meeting in Ipswich, city council member Mike Hammrich said the hope was to buy and operate the home through a nonprofit organization.
Hammrich said Ipswich residents had just three and a half weeks to raise the money, and could not do so. About $170,000 was raised, but at least $250,000 was needed to buy the nursing home, and more money was needed to run it, he said.
Hammrich praised the community effort, adding that Avantara was helpful and walked them through the process. “We gave it one heck of a shot,” Hammrich said.
— Reporting by Alexandra Hardle, Aberdeen News
The 2021 inspection report gave examples of serious deficiencies in resident care at Avantara Ipswich. Some residents lost large amounts of weight; others were found by family members to be frequently soaked in urine; some had injuries or ulcers that were not documented or treated; and one elderly man had catheter problems that caused his penis to begin “eroding away.”
The pending closure of the home in Ipswich is an ominous sign for the state’s nursing home industry, which is a critical component of the healthcare continuum in South Dakota and a basic necessity for many of the state’s oldest and most vulnerable residents, said Mark Deak, director of the South Dakota Health Care Association. Deak was not directly familiar with what has taken place at Avantara Ipswich, but he said the inability of nursing homes across the state to hire workers was a problem even before the pandemic.
“For something as critical as long-term care, this is a big deal,” Deak said. “The issue is particularly acute in the rural areas.”
Lack of revenue a hurdle for homes
Beyond staffing challenges, providing consistent, adequate funding of nursing homes remains a related and ongoing issue. For each resident on Medicaid, the federal health plan for low-income residents, nursing homes lose more than $50 per day, according to state and federal documents. That equation means the roughly 100 nursing homes in South Dakota lose about $56 million a year combined in unreimbursed care provided to Medicaid recipients, who make up about 55% of the overall residents in nursing homes.
The heightened concerns over viability of nursing homes comes after a disastrous year in 2020-2021, when the pandemic hit. Nursing home employee costs rose by about $30 million overall that year in South Dakota, while revenue fell by an estimated $60 million due to heightened virus protocols and reduced admissions.
The South Dakota Legislature, recognizing the funding crisis, allocated in the 2022 session about $30 million in one-time funding to temporarily boost the bottom lines of nursing homes. The funding, which will reach nursing homes before June 30, 2022, equals about a 20% bump in annual state funding to nursing homes, according to a legislative budget memo.
In the memo, the Joint Committee on Appropriations said nursing homes could use the state money to raise employee pay, but the committee urged the recipients to spend the resources on “business continuation efforts” and “to use them for one-time expenses such as construction, debt payment or retention bonuses.”
Deak said the cash infusion is needed, but not adequate in the long run to stabilize the long-term care industry. “That will help float some people for a while, but that is also just a Band-Aid,” he said.
Despite the one-time state funding bump, and incremental increases in Medicaid funding in recent years, South Dakota remains near the bottom of all states in regard to state Medicaid reimbursement levels.
Deak said that without a more stable funding source, and an increase in the ability of homes to hire and retain healthcare workers, the industry may continue to suffer closures and overall constriction even as the need for long-term care is expected to rise dramatically in coming years.
South Dakota saw a handful of nursing home closures, mostly in rural areas, over the past five years.
Each time a home closes, it upsets the lives of many people, said Erica Larson, a city council member in Ipswich.
“That will definitely hurt our small town, for those employees and those families that have loved ones in our facility,” Larson said. “When people come to visit, they stop in our town and visit our grocery store and convenience stores. It will definitely hurt us a lot by not having the people come here and spend money in our local facilities and by not having our loved ones here in the community.”
Deak said the combination of insufficient workforce, rising business and personnel costs and stagnant or barely rising revenues could lead to serious repercussions in the long-term care industry in South Dakota.
“What’s been happening, and this is a very tough situation, is they don’t take new admissions; they simply do not have the staff to take on new residents that need their care,” Deak said. “And without taking on enough residents, obviously that hurts the viability of their operation, so it really catches them that way and makes it very difficult.”

"What’s been happening, and this is a very tough situation, is they don’t take new admissions; they simply do not have the staff to take on new residents that need their care." -- Mark Deak, executive director of the South Dakota Health Care Association
Tough job, low pay, but big rewards
Healthcare workers of all sorts remain in great demand in South Dakota, where wages are generally lower than in other states.
Among the most difficult positions to fill, and among the most critical in terms of function, is the certified nursing assistant position.
According to the state Department of Labor and Regulation, the nurse aide position will be one of the fastest-growing professions in the state over the next decade, with employment of almost 4,000 by 2028, if open positions can be filled.
But becoming a CNA requires education, training and expertise not demanded of entry-level workers in other fields, who can often make more money per hour.
A survey of South Dakota nursing homes in 2021 showed the average pay for a CNA was $14 an hour, or $29,000 a year. Many fast-food workers are being hired for higher pay in the current employment market, and they don’t have to manage elderly residents, provide them food, bathing and bathroom assistance, or go through the extensive training required of CNAs.
To become certified, CNAs must be at least age 16 and complete 75 hours of classroom and clinical instruction. They then must pass a written or oral final exam and complete a competency evaluation that includes performing at least five nursing tasks on a live person. Nursing aides must also undergo 12 hours of training annually to maintain certification.
About three dozen individual skills are required for certification, including basic duties such as communication and interpersonal skills, taking and recording vital signs, height and weight, and showing proficiency in feeding, bathing, dressing and toileting of patients.
But CNAs must also be proficient in more medically sensitive skill areas, including: infection control; overseeing range of motion and use of prosthetics or orthotics; using mechanical lifts; completion of several reporting and security functions; caring for patients lacking bladder or bowel control; handling patients with dementia or cognitive decline; and caring for patients when death is imminent.

The Evangelical Lutheran Good Samaritan Society, which runs 23 housing campuses in South Dakota, many of them with nursing homes, is taking aggressive steps to recruit and retain more healthcare workers, said Rochelle Rindels, vice president of nursing and clinical services at the agency.
As of mid-April, Good Sam had about 1,000 nursing employees but about 250 open positions in South Dakota, including 65 openings for licensed nurse positions and about 180 CNA openings.
CNA jobs remain hard to fill in South Dakota, where overall job openings are plentiful and the available workforce is low. Furthermore, working as a CNA is a difficult job that requires a great level of caring and commitment, Rindels said.
“They come in at that entry-level pay, and it’s a very physical job,” she said. “If somebody comes into the position and doesn’t really expect what the work would be or look like, it can lead to burnout.”
Long-term care facilities have a hard time competing with other entry-level industries, such as manufacturing or service industries, which can raise employee pay and then pass that cost on to consumers, Rindels said. Nursing homes are limited in how much they can charge before pricing customers out of the market, and Good Sam, like most providers in South Dakota, has about half its residents on Medicaid, which provides a set per-resident funding level each year.
Good Sam is working to become more competitive on pay, especially for CNA positions, recently investing $15 million targeted at raising pay for healthcare employees. Last year, the agency developed a new program to recruit and pay to train people interested in the CNA position, Rindels said. So far, about 600 students have entered the program and more than 90% have made it through and passed state certification exams.
Rindels said additional training programs, new funding sources and expanded employee-support systems are needed on the federal and state levels to stabilize staffing at nursing homes in South Dakota.
“We’ve got to continue to invest and find some creative solutions to ensure that the workforce is there to provide care, to partner with state and federal associations to really just come at this staffing challenge from multiple perspectives,” she said. “It’s a challenge, but it’s extremely important in our state to provide care for people close to home.”
Rindels said she and other lifelong nurses often feel a calling to the profession and greatly value the opportunity to help people, to provide high-quality medical care and to build positive, long-lasting relationships with residents, families and staff.
“It’s the relationship and the friendships that you build,” she said. “It’s the things you learn and the wisdom shared by residents, and attending all those birthdays and anniversaries.”
Deak said the nursing home industry will continue to struggle to find workers if it cannot even compete with entry-level pay at fast-food outlets. Deak, who spent a day following a CNA a few years ago, has a deep appreciation for how difficult the job can be.
“It takes a particularly special person, someone with angelic qualities, to do the day-in and day-out hard, physical and emotional work of working in a nursing home,” he said. “If Taco Bell is hiring for a couple bucks more an hour, it might be worth it for the extra money and easier work, too.”
He added: “We’re really looking for angels and they’re tough to find sometimes, and they need to put food on their tables at home, too.”
Deak said the long-term care industry may need to look to more immigrant laborers to fill the many open positions. He also suggested that perhaps immigrants from Ukraine, fleeing the war in their country, could help fill employment gaps at South Dakota nursing homes.

“We’ve got to continue to invest and find some creative solutions to ensure that the workforce is there to provide care ... it’s a challenge, but it’s extremely important in our state to provide care for people close to home.” -- Rochelle Rindels, vice president of nursing at Good Samaritan Society
A troubling inspection in Ipswich
Some of the deficiencies noted by state inspectors during their April 2021 inspection of Avantara Ipswich involved a lack of basic procedures such as developing “care plans” for all residents, implementing a toileting plan for all residents and not properly documenting skin conditions and other ailments. Low morale and operational confusion within the staff were also noted in the report.
Other deficiencies found by inspectors included unsafe or unsanitary conditions for residents.
One female resident went from 152 pounds to 133 pounds in three weeks, and the rapid weight loss was not documented by staff or reported to a physician. Another resident was given the wrong dose of a vitamin.
Residents were not provided adequate care for incontinence, the report stated. One female resident said bedpans were left in too long and became painful. One resident was sent to the emergency room, where nurses found two skin tears, a bruise and an ulcer on the perineum that had not been documented or addressed by employees at the home, according to the report.
The treatment of one man was the subject of a lengthy analysis. The man’s wife said she found him regularly soaked in urine and with dried urine under his bed, dried food on the floor and a soiled trash can. His wife reported that his legs were red, swollen and oozing and that he had an undocumented open sore on his buttock. The day after Christmas 2020, the resident was found to have removed a problematic catheter and after he arrived at an emergency room, his penis was found to be “eroding away,” the report stated.
“There was no other communication or notes regarding resident’s penis eroding away. There was no communication regarding the open sore on his buttocks,” the report noted.
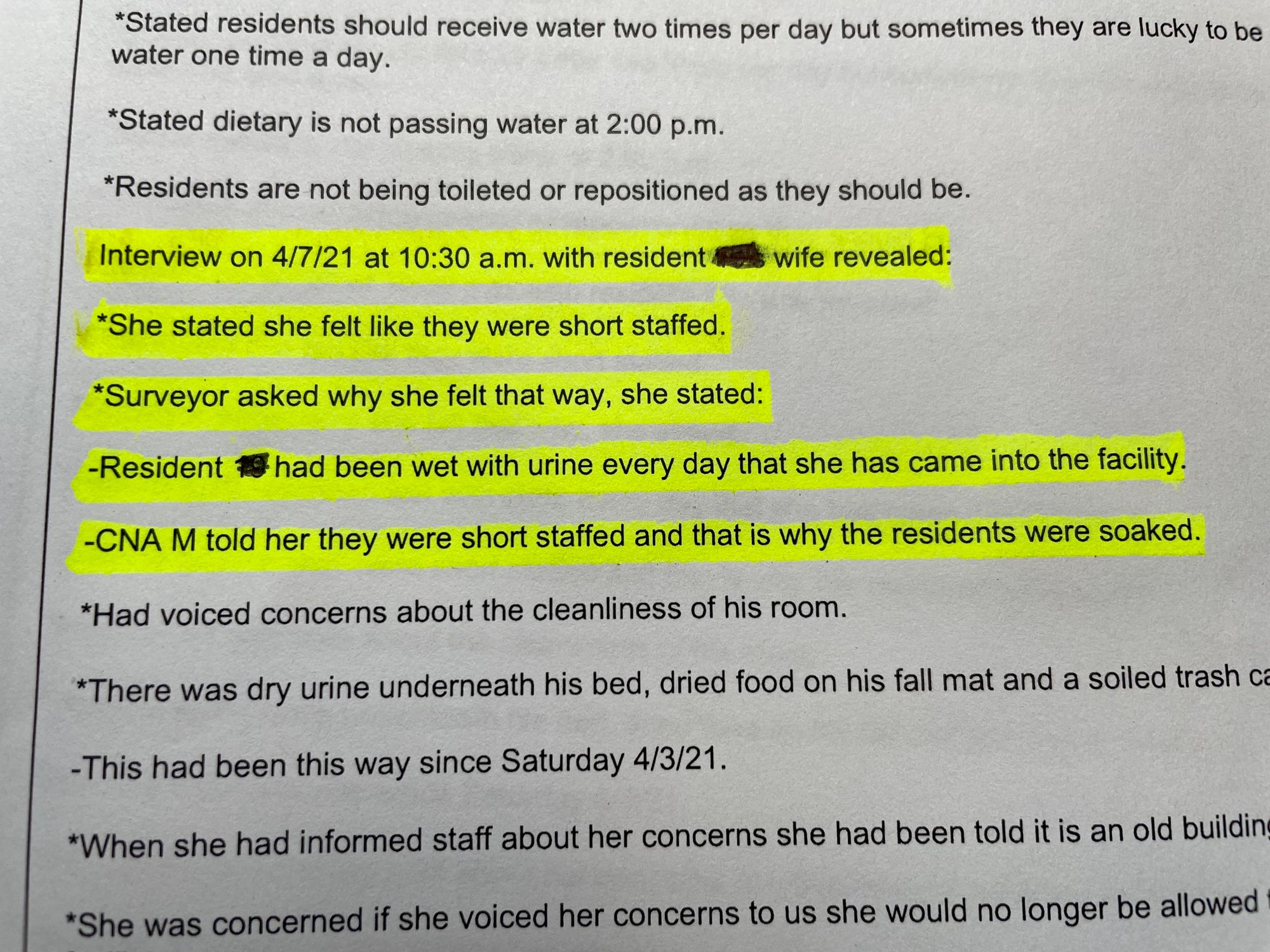
Another man, a 75-year-old Vietnam War veteran, lost 18 pounds in three weeks and was also frequently found by his wife to be out of water and wearing urine-soiled clothing.
That resident’s wife told inspectors that nursing home staff said her husband was “naughty, naughty, naughty” during clothing changes and that closer monitoring of his water intake would be “entirely too much work.”
In several areas, the inspection report pointed to a lack of staffing as a primary cause of deficiencies in care at the Ipswich home.
“The provider failed to ensure sufficient nursing staff were available at all times to provide nursing services to meet residents’ needs safely and in a manner that promoted each resident’s rights and physical, mental, and psychosocial well-being,” the report stated.
Inspectors found that the activities director was sometimes forced to serve as a nursing assistant.
An inspector, called a surveyor in state reports, also interviewed the clinical care coordinator of the facility in April 2021 and noted the coordinator was also serving as interim director of nursing at the time.
“When surveyor asked who was in charge of infection control for the facility, she stated, ‘I guess that would be me,’” according to the state report.
The coordinator also told the inspector that infection-control matters, even during the COVID-19 pandemic in 2021, were “not really” part of the discussion at quality-assurance meetings.
“Surveyor asked who was in charge of antibiotic stewardship for the facility. She stated, ‘probably me,’” the report noted.
The coordinator was not sure whether a physician or pharmacist was involved in the facility’s antibiotic-stewardship program.
Followup reports from the state indicate that the deficiencies found in the April 2021 inspection had been fixed. The 2021 inspection found far more deficiencies than inspections in October 2019, when seven deficiencies (two related to quality of life and care) were found, and in August 2018, when three deficiencies were noted (only one related to quality of life and care,) according to state records.
In the press release announcing the pending closure of the nursing home, Legacy Health Care official Connie Ortega said the decision to close Avantara Ipswich was difficult, but that “the challenges related to staffing and the continued impact of COVID-19 have created an environment where we can no longer keep the doors of Avantara Ipswich open.”
Residents and their families will be given individual plans to relocate and continue their care, the release said.
The release praised the staff at Avantara Ipswich as “incredibly hardworking and dedicated to the care of our residents and community” and said the company would help employees explore other opportunities.
The release said Legacy made significant investments into the home and had worked with state officials to find solutions. The home has filed a formal closure notice with the state, the release said. Other Avantara nursing homes operated by Legacy Health Care in South Dakota are located in Arlington, Armour, Clark, Groton, Huron, Lake Norden, Milbank, Pierre, Rapid City, Salem and Watertown.






