South Dakotans battling addiction to opioids are increasingly relying on medication-assisted treatments to overcome their cravings for the dangerous drugs and to avoid potentially deadly overdoses.
However, access to the life-saving medications is limited in South Dakota and some physicians in the state are reluctant to prescribe the drugs that have shown great promise in overcoming opioid abuse. Meanwhile, addiction experts and some law enforcement officials are trying to break down barriers to wider use of the treatments.
Medication-assisted treatments for addiction use drugs approved by the U.S. Food and Drug Administration to alleviate withdrawal symptoms and relieve cravings resulting from chemical imbalances in the body. As the prescription drug treatments take effect, physical symptoms of addiction will ease, allowing patients to focus on work, relationships and their health. The medications can be taken on a short-term or long-term basis and are increasingly viewed as a successful method of improving the lives and health of people addicted to opioids.
Opioids are a class of addictive drugs that include the illegal drug heroin, synthetic opioids such as fentanyl, and pain relievers legally available by a prescription. Opioids, which have devastated thousands of lives in other states, are not the most widely misused drugs in South Dakota but they are responsible for a majority of fatal overdoses, according to the Centers for Disease Control and Prevention. Nationally, 70% of all overdose deaths involve an opioid.
While the treatment has been available for decades, access to medication-assisted treatment has gained traction in South Dakota only within the past five years. More than 90,000 drug overdose deaths are estimated to have occurred in the United States from September 2019 to September 2020, the highest number of overdose deaths ever recorded in a 12-month period according to the CDC. Opioid fatalities increased by 55% over the previous 12 months.
South Dakota experienced a more than 20% increase in all drug overdose deaths from 2019 to 2020, according to an emergency health alert from the CDC in December. About half of the 38 states that track synthetic opioid overdoses reported an increase of at least 50% in those overdose deaths from 2019 to 2020, according to the report. The largest increase in opioid abuse was seen in rural counties in western and midwestern states.
Medication-assisted treatment is considered the most effective way to treat addiction, known as opioid use disorder. Evidence has shown medically supervised withdrawal from opioid addiction is safer than the abstinence-only, or cold turkey approach, according to Avoid Opioid SD.
About 90% of patients who receive the treatment remain free from addiction for more than two years, according to the FDA. Nearly 100% of all people who solely go to traditional drug treatment or rehabilitation will relapse, and many overdose because of misjudged tolerance within six months of release.
“A lot of patients have told us it saves their life,” said Dr. Dan Felix, a licensed mental health therapist and director of behavioral health at the Sioux Falls Family Medicine Residency program. “It prevents overdose and relapse. We take a de-stigmatized approach to treatment. Come and be the human that you are.”
Janine Crowe, a 35-year-old resident of Sioux Falls, was addicted to opioids for more than a decade and could not shake her addiction until she began a treatment plan that included medications to ease her cravings for painkillers.
“It helps me stay sober,” said Crowe. “It helped with my anxiety. It got me out of the mind frame of using drugs.”

Medication-assisted treatment can be provided by physicians, physician assistants and nurse practitioners who undergo additional training to be certified with what is called an “X Waiver.” Counseling and other care services are usually part of the overall treatment plan, but the medication itself is effective in curbing cravings, Felix said.
Methadone, an opioid, has been used to treat addiction to other opioids for more than 50 years, but it is potent and can only be taken through certified programs. The only facility in South Dakota that can dispense methadone is the Sioux Falls Treatment Center.
Buprenorphine is a more common, safer alternative. It partially activates opioid receptors in the rain, often reducing drug use and protecting patients from overdose by reducing cravings. Buprenorphine, which can be prescribed by a primary care physician, does not put patients in the euphoric and impaired state that makes opioids ripe for abuse.
Some critics of the treatment say it is simply “trading one addiction for another,” creating a difficult-to-change negative stigma around addiction treatments that some patients and doctors still cling to, Felix said. That thought can keep patients from seeking help or keep doctors from providing the treatment.
“This is replacing one drug for another; it’s replacing one that’s going to kill you for one that’s going to save your life,” Felix said. “People are dying from this epidemic, and we have an amazing cure, yet people are stigmatizing it.”
Over the past five years, millions of dollars in federal and state funds have been used to train more health care providers to prescribe appropriate levels of pain medication to avoid addiction. Prevention efforts have been made to educate the public and providers on the potential for opioid abuse.
Between June 2019 and May 2020, the Center for Family Medicine provided MAT education to 58 medical providers or medical students in South Dakota, 10 of whom eventually obtained waivers required to administer the opioid treatment medications. Each year, about 14 pharmacy students in the state receive the training.
As part of Avera Health’s Project ECHO — Extension for Community Healthcare Outcomes — the Center for Family Medicine has provided training to providers from 66 different health care facilities.
More than 950 people have begun a medication-assisted treatment program at one of the three MAT providers in South Dakota, including the Center for Family Medicine, Project Recovery and Lewis and Clark Behavioral Health, according to the 2020 annual report from the state-led Opioid Abuse Advisory Committee. The committee, formed in 2016, has used more than $24 million in federal funding to expand education and prevention, increase access to treatment, improve data collection and decrease the overall opioid supply across the state.
Even with these efforts, advocates say addiction care is still insufficient in South Dakota.
“South Dakota is kind of behind in its addiction care,” said Dr. James Wilde, who leads the Center for Family Medicine addiction care team. “They don’t treat the underlying reason for why people overdose.”
Medication-assisted treatment was made more available last year during the pandemic when the Drug Enforcement Administration allowed providers to prescribe the medications to patients virtually. Normally, patients must be seen in person before being prescribed one of the medications to treat opioid addiction.
That flexibility will likely end when the State of Emergency surrounding the pandemic ends, reinstating a geographic hurdle for addiction patients in rural South Dakota, where care was and is still not as widely available.
In 2016, only about 12 of South Dakota’s 66 counties had at least one health care provider who could prescribe the most-used medication to treat opioid use disorder, buprenorphine, according to the Federal Office of Rural Health Policy. Nationally, fewer than 1 in 10 people have access to this type of care.
“MAT is the gold standard for opioid addiction treatment,” said Dr. Stephen Tamang, a family physician for Monument Health and founder of Project Recovery in Rapid City. “When I started (practicing), there was a big dearth of access here. There were no significant services at all.”

Project Recovery, the state’s largest telehealth addiction recovery program, was founded in 2017. It has experienced rapid growth in service requests each month over the past year, Tamang said. Project Recovery can diagnose addiction and prescribe medication to patients via telemedicine and provides services to some tribal communities across the state, including those on the Pine Ridge Indian Reservation.
The number of prescriptions doctors give for opioids as a painkiller has been on the decline since 2012, but use and overdoses have been on a steady increase, mostly because of illegal manufacturing and selling. Some drugs sold on the streets are laced with powdered fentanyl, a substance up to 100 times more potent than morphine and usually mixed with other opioids to stretch supply. Humans can die from just 2 milligrams of fentanyl, equivalent to a few grains of salt, according to the DEA.
“This is replacing one drug for another; it’s replacing one that’s going to kill you for one that’s going to save your life. People are dying from this epidemic, and we have an amazing cure, yet people are stigmatizing it.” -- Dr. Dan Felix of the Sioux Falls Family Medicine Residency program
Law enforcement across South Dakota is seeing more fentanyl in illegal opioid sales. When someone seeking the opioids purchases pills illegally, they could be getting a more potent substance than they expect and accidentally overdose. Law enforcement seized 312 grams of fentanyl in South Dakota in 2020, according to the DEA. That equates to about 156,000 lethal doses.
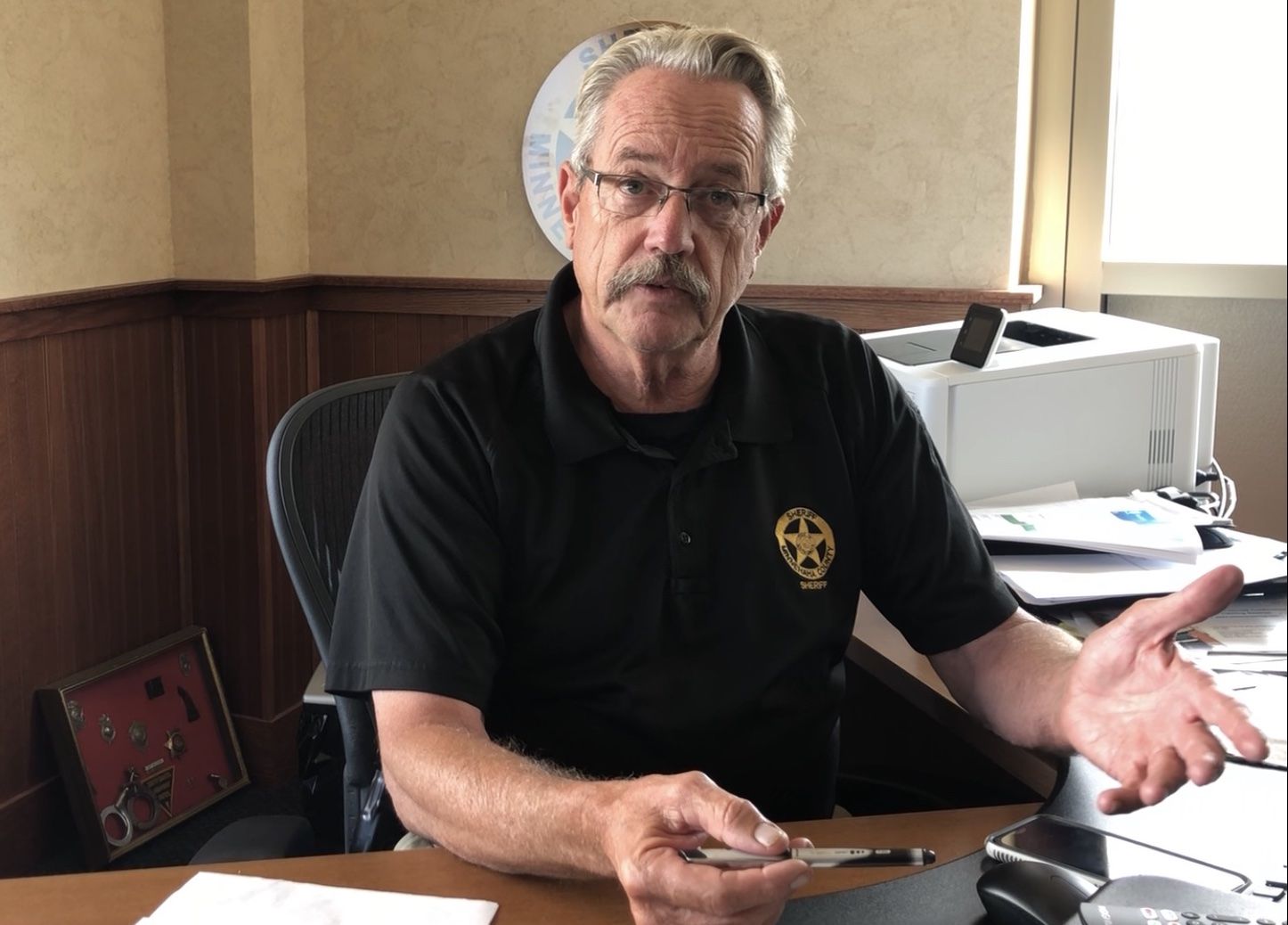
“A lot of those overdose deaths are attributed to opioids, fentanyl,” said Minnehaha County Sheriff Mike Milstead. “That has a huge impact on people’s lives and families. A lot of the time, these people aren’t trying to kill themselves. These are accidental overdose deaths. It really raises to the level of recognizing it’s a serious problem.”
The Minnehaha County Jail will soon become the first facility in the state to treat inmates with opioid addiction medications after they arrive. The jail has allowed inmates who are already on the treatment to continue it, and has long allowed pregnant women to start or continue the treatment. Previously, the Yankton County Jail was the only jail that allowed patients to continue on the treatment, according to the Center for Family Medicine.
Everyone who gets booked into the Minnehaha County Jail is screened, said Warden Mike Mattson. There, health care providers can identify who is already on the treatment and who may qualify to start. Once someone is released, case managers will connect them to outside services in the community, Milstead said.
“They’re not always Minnehaha County residents,” Milstead said. “Fortunately, MAT is expanding the state so we can connect them with more [services] across the state.”
Having the treatment in the jail is an opportunity to get help to people who don’t normally have access to health care or other basic needs, and provide treatment when they are away from opioids, said Michelle Boyd, Minnehaha County programs and services coordinator.
“The best time to get you into a program and your brain healing is when you don’t have access to the drugs,” Boyd said. “Being able to get them started on treatment so they can start to feel healed gives them that little boost. Once their head clears and they want their family back, that’s the best time that you can give them a good start.”
Boyd said she has noticed a recent increase in the number of participants who use medication-assisted treatment and expects that number to continue to rise.
Crowe, the Sioux Falls resident, is now in her last phase of drug court. She heard about medication-assisted treatment through other women who were also staying at the New Start treatment center.
“I said, ‘I don’t know if I can take this anymore,’” Crowe said. “They said, ‘Why don’t you try medication?’ I said, ‘There’s medication?’”

Crowe’s addiction to pain pills and methamphetamine started in 2008, after her husband was killed by a relative on the Crow Creek Indian Reservation. She sought mental-health care at an Indian Health Service clinic, but was not provided antidepressants, she said. She sought comfort at a relative’s home. That relative gave her the opioid Darvocet to manage pain from an infected ingrown toenail and Crowe enjoyed the euphoria that came with the pain relief.
“One thing led to another,” she said. She went on to try tramadol and eventually moved to oxycodone and methamphetamine.
“I craved them bad,” she said. “I woke up and thought about them.”
She completed six months of traditional treatment, but relapsed shortly after being released.
“My heart was in it, but I couldn’t get the drugs off my mind,” she said. “Everything you do is drug-related. The reason you get up is because you’re going to look for a drug. Your body language, you’re sweaty, you get shaky, kind of like the flu feeling if you don’t get it.”
She was nervous to try the medication-assisted treatment, but she said it was her “last option.”
She went to Falls Community Health and was given Suboxone in the form of a tablet that dissolves under the tongue. Within hours, she noticed her cravings cease and didn’t feel the flu-like withdrawal symptoms she would normally feel if she went without using.
“I didn’t want tramadol anymore,” she said. “I didn’t crave anything. A weight was lifted off my shoulders. It was a relief. I take one tablet three times a day.”
Crowe now has a job, an accomplishment she would have thought unobtainable two years ago.
“I used to be on the streets, never held a job,” she said. “Now I work. I’ve been sober for almost two years now.”
How to find help for addiction
Here are some options to find medication-assisted treatment and other addiction services in South Dakota.
Avoid Opioid SD: https://www.avoidopioidsd.com/
Lewis and Clark Behavioral Health, Yankton:
Phone: 605-665-4606 or toll free 1-800-765-3382
Website: https://lewisclarkb.yankton.multisiteadmin.com/
Center for Family Medicine, Sioux Falls:
Phone: 605-575-1637 to schedule with Cindy, substance use nurse case manager
Website: https://centerforfamilymed.org/
Project Recovery, Rapid City:
Phone: 605-340-1234




